Robotic-Assisted Radical Prostatectomy (RARP)
This page is to provide you and your family with information regarding your treatment and recovery from a robotic assisted radical prostatectomy. It explains why this operation may be suitable for you and what you can expect. It also outlines the advantages, possible risks and the most common questions raised by patients.
What is a robotic assisted radical prostatectomy?
A robotic-assisted radical prostatectomy is an operation to treat localised prostate cancer (cancer that has not spread outside the prostate gland). It is performed under a general anaesthetic, which means you are asleep for the whole procedure. Six small incisions are made into the abdomen to insert key-hole instruments.
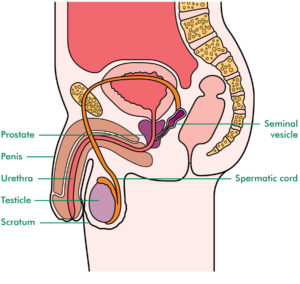
The operation involves removing your prostate gland, seminal vesicles (glands that store semen), and possibly surrounding lymph nodes. The urethra (tube that carries urine from the bladder out of the body) is then re-attached to your bladder.
What happens before my operation?
Before your operation you will attend an outpatient’s appointment. It is important that you attend this appointment. At this appointment you will need to fill out a ‘Health Assessment Questionnaire’. The registered nurse in the clinic will discuss your general health and the answers you have provided in the questionnaire. You will also need to attend the pre-admission clinic for an appointment with a member of the Anaesthetic team.
You will be required to have routine blood tests and have an ECG tracing of your heart before your operation.
At the Pre Anaesthetic Clinic the anaesthetist will review the results of your blood tests and your ECG; discuss with you your preferences and decide the type of anaesthetic which is best for you.
Please notify the anaesthetist and your surgeon if you are on any medications, especially anticoagulants (blood thinning medications). You will be given instructions about stopping these medications before your operation and instructions about when you can start taking them again.
Your nurse specialist will discuss the details of the procedure with you before your operation. You may also be shown a video of the procedure if you wish.
If you smoke, you should try to stop as long before surgery as possible. Smoking increases the risk of developing complications following surgery, such as a chest infection. It can also delay wound healing. Remember- every smoke free day helps. For help in giving up smoking, please speak to your nurse.
On the day of your surgery
You must not eat or drink for 6 hours prior to going to the operating theatre for your operation.
The nurses will advise you of the appropriate time to stop eating and drinking before your operation.
On arrival to the hospital you will be required to register on the ground floor of the ATC. Following completion of your admission forms you will then be taken to the surgical reception.
The surgical reception staff will show you to your bed space. They will check your details and ask you some questions. You will be asked to change out of your clothes into a gown. The anaesthetic and surgical teams will come and see you before you go to theatre. Any friends and family members can leave the hospital or wait within the hospital.
You will be taken on the bed to the anaesthetic room/operating theatre, where you will be seen by the anaesthetic nurse and doctors. They may put a drip into your arm to for some fluids and medications during the operation. Once anaesthetised, you will be taken through to the operating theatre. The operation usually lasts two to four hours.
What are the possible risks of a robotic assisted radical prostatectomy?
Robotic assisted radical prostatectomy is major surgery, but it is generally very safe. Your consultant will discuss the risks listed below with you in more detail, but please ask questions if you are uncertain:
Problems during surgery or in hospital
Problems relating to the general anaesthetic: These include chest infection; deep vein thrombosis (DVT); a pulmonary embolus (blood clot in the lung); stroke; or heart attack. These are rare.
Blood loss: Severe bleeding may require a blood transfusion or another operation. This occurs in approximately 2% of cases.
Injury to your bowel or rectum: Very rarely (less than 1%) there may be injury to your lower bowel during surgery. Sometimes a temporary colostomy may be required to improve healing.
Wound problems: Infection or hernia can occur at the wound sites.
Death: This is very rare. Approximately 3 in 1000 of patients die from complications of surgery.
Problems after leaving hospital
Urinary incontinence: Short term urinary incontinence is common. Continence recovers within a few weeks or months for most patients, and can be helped by performing pelvic floor exercises. 5-10% of patients continue to wear pads after one year, and 1-2% undergo further surgery to treat the problem.
Urine leak: Occasionally, when the catheter is removed the join between the bladder and the urethra may leak. This can cause some discomfort, and the catheter may need to be reinserted for another week or so.
Bladder neck/urethral scarring: occasionally (about 1%) a narrowing of the urethra or the neck of the bladder can occur in the months after surgery. A further minor operation may be required to correct it.
Erectile dysfunction: Some erectile dysfunction is inevitable after prostatectomy. Recovering your erections can take up to two years and will depend on a number of factors.
Positive margin: This is when cancer cells are found at the edge of the removed prostate tissue, and suggests that there may be cancer cells remaining inside. The results of the operation will be discussed at your first appointment after surgery.
Rise in PSA level or recurrence of prostate cancer: It is important to note that some men, despite a successful operation, may get a rise in the PSA blood test in the months or years following surgery. In some cases further scans or treatments may be necessary.
What should I expect after my surgery?
A catheter: The catheter will be left in place for approximately 7 days following surgery to allow the join between your bladder and urethra to heal. Once you are walking a smaller bag will be attached to your catheter that you can strap to your leg.
Stitches closing your wounds: these dissolve and do not usually need to be removed.
Pain: You should take regular pain medication for a few days after surgery. Most men do not need strong pain relief after the operation.
Mobility: You should sit out of bed and walk around within a few hours of surgery. You should only get back into bed at bedtime or to take a nap. This is important for your circulation, breathing and bowels. It will help you to pass wind, which will make you feel a lot more comfortable.
Leaving hospital
90% of patients go home the day after their surgery. Your urology team will visit you on the ward before you leave to make sure you have an appointment for your catheter to be removed.
What can I expect when I get home?
Tiredness: You should not forget that you have had major surgery.
Bowels: You may not open your bowels for a few days, which is normal. Use regular laxatives when you get home for a couple of weeks to help open your bowels without having to strain.
Catheter: You might get some blood or urine draining around the sides of your catheter. This is normal. Your bladder is not used having the catheter tube in place. Carry out twice-daily catheter care to help reduce the risk of infection. If you become very uncomfortable, contact your urology nurse who will give you advice.
Diet: Eat a light, soft diet until your bowel movements are back to normal
Exercise: Regular, gentle exercise such as walking will help to prevent complications after your surgery. Do not lift anything heavy or do anything too energetic (for example, shopping, mowing the lawn, lifting weights or running) for at least two to four weeks
Work: Take at least two weeks off before returning to work, maybe more depending on the type of work you do.
Driving: Only start driving again when you are able to perform an emergency stop without feeling hesitant in doing so. Check with your insurance company to make sure you are covered to start driving again. Some pain medications cause drowsiness. If you are taking painkillers, please check with the pharmacist whether it is safe to drive.
Wounds: You should wait 2-3 days before showering, and a week before having a bath, or swimming. Until that time you can have a flannel wash.
Your catheter removal
Your catheter will be removed by a specialist nurse in our clinic approximately 7 days after your surgery. The specialist nurse will then monitor you for the next few hours to make sure you are able to pass urine. Removing the catheter is straightforward, so please do not worry.
You will receive a follow up phone call to ensure you are passing urine
It is normal to have some urinary incontinence after having the catheter removed. You will need to wear a pad for the first few months following removal of the catheter. Do not feel embarrassed, almost all patients have this experience.
You need to regularly practise your pelvic floor muscles. These exercises strengthen the muscles and help with regaining your continence. We recommend that you start the pelvic floor exercises as soon as your catheter is removed and repeat them every day. Your nurse will give you further advice to the frequency required.
When can I have sex again?
You may start sexual activity again two weeks after your operation, as long as you feel comfortable. You will not be able to achieve an erection in the early stages of your recovery, but you can experience arousal and even climax without an erection.
After surgery it will more difficult for you to have an erection than it was before your surgery. We can offer you treatment, such as medication, to help restore your erectile function. We will start you on tablets to aid erections after your catheter is removed.
Your penis may look shorter following surgery. The penis can be stretched out, which will help restore the length. Please speak to your nurse specialist for more information.